Reviewed by Dr Reza Lankarani, General Surgeon
Founder | Surgical Pioneering Newsletter and Podcast Series
Editorial Board Member | Genesis Journal of Surgery and Medicine
These sources summarize prominent surgical research and academic analyses scheduled for publication in 2025, primarily from the JAMA Surgery and the Briti
sh Journal of Surgery. The collection highlights technological advancements in the field, such as the use of novel fluorophores for nerve visualization and the efficacy of robotic-assisted procedures. Several clinical trials evaluate postoperative recovery strategies, comparing the performance of synthetic versus biological meshes and testing personalized prehabilitation programs for frail patients. Beyond clinical data, the documents explore historical perspectives on surgical tools, methodological guides for big-data research, and practical advice for surgeons seeking patents. Collectively, these articles establish new benchmarks for quality
improvement and evidence-based standards across various minimally invasive and oncological specialties.

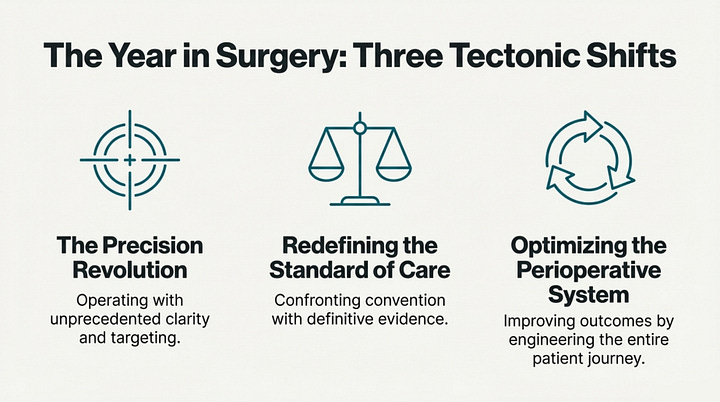
Introduction: Question Everything You Think You Know About Surgery
Medicine is a field of constant evolution. What is considered standard practice one day can be challenged and overturned by new evidence the next. Long-held beliefs and "common sense" assumptions about what works best in the operating room are continuously put to the test by rigorous scientific research. It is through this process—the willingness to question, test, and adapt—that true progress is made.
This article explores five of the most surprising, counter-intuitive, and impactful findings from top surgical journals in 2025. From the hidden risks of advanced robotics to the dramatic failure of a "natural" alternative, these studies challenge our assumptions and are actively changing the future of surgery.
The Five Most Surprising Surgical Findings of 2025
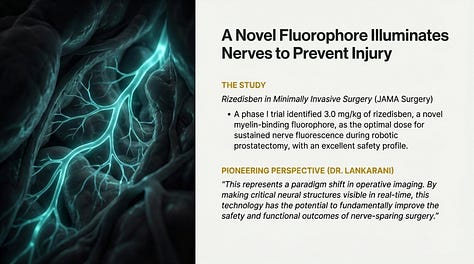
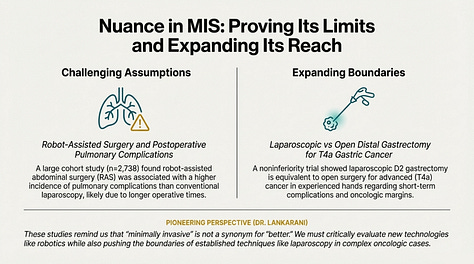
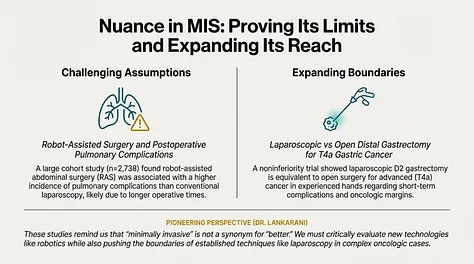
Finding 1: The 'Better' Robotic Surgery Has a Hidden Risk. The widespread perception of robot-assisted surgery is that it represents the safest, most advanced, and superior form of minimally invasive procedures. The precision and enhanced visualization offered by robotic platforms have made them an increasingly popular choice for a wide range of operations.
However, a large international cohort study of 2,738 patients delivered a counter-intuitive finding: robot-assisted abdominal surgery was associated with a higher incidence of postoperative pulmonary complications compared to conventional laparoscopic surgery. The study identified the longer duration of the procedure under anesthesia as the primary driver of this
increased risk.
This finding provides a crucial piece of real-world evidence that challenges the assumed superiority of robotic platforms in every scenario. It doesn't negate the benefits of robotic surgery, but it underscores the critical importance of optimizing operative time and refining anesthetic and ventilation strategies during these longer procedures. This forces a more nuanced conversation about when and how robotic platforms should be used to ensure the best possible patient outcomes.
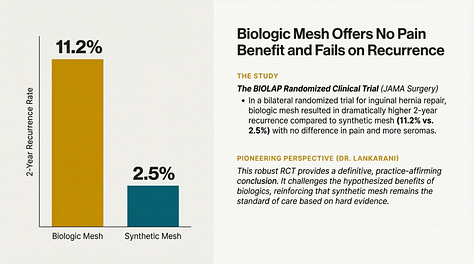
Finding 2: The 'Natural' Choice for Hernia Repair Was a Dramatic Failure
Inguinal hernia repair is one of the most common surgical procedures performed worldwide. In recent years, the idea of using a "biologic" mesh derived from animal tissue has held an intuitive appeal. The logic was that a more natural, absorbable material might integrate better with the body and cause less long-term pain than a permanent synthetic mesh.
The BIOLAP randomized clinical trial put this logic to a direct, head-to-head test with stunning results. In this trial, 491 patients received both mesh types and were followed closely. The study found that the biologic mesh offered no advantage in postoperative pain. More alarmingly, it resulted in a dramatically higher rate of hernia recurrence at the two-year mark—11.2% for patients with biologic mesh versus just 2.5% for those with synthetic mesh.
The verdict from the medical community was decisive, as synthesized in the study's editorial commentary:
These results decisively counter the hypothesized advantages of biologics, reinforcing that synthetic mesh remains the undisputed standard of care based on robust, head-to-head evidence.
Finding 3: A Good Idea Isn't Enough—Execution Is Everything
The concept of "prehabilitation" is both logical and well-intentioned: why not strengthen frail, older patients before a major operation to help them recover better afterward? This approach aims to build up a patient's physiological reserve to better withstand the stress of surgery
.But does it work? The evidence from 2025 is mixed and reveals a crucial lesson. One rigorous, multicenter trial of a coach-supported, home-based program for frail older adults found that it failed to improve primary outcomes compared to usual care. In contrast, another trial that tested a personalized prehabilitation regimen found measurable benefits, including improved immune parameters and slightly better functional recovery.
The lesson isn't that prehabilitation "doesn't work," but that how we implement it is critical. These studies suggest a one-size-fits-all approach may be insufficient for vulnerable patients, while a tailored, personalized intervention shows real promise. It's a powerful reminder that in medicine, good intentions must be backed by data, and execution is everything.
Finding 4: Minimally Invasive Surgery Is Now Ready for Advanced Cancer
A core surgical assumption has long been that advanced cancers—like a T4a gastric cancer that has grown through the stomach wall—require a large, open incision. The traditional belief was that only an open approach could guarantee the visibility and access needed to remove the entire tumor safely and completely.
The UMC-UPPERGI-01 trial directly challenged this dogma. Researchers compared laparoscopic versus open surgery for these advanced gastric cancer cases and found that the short-term outcomes were statistically equivalent. This included key metrics like 90-day complications and, most importantly, oncologic clearance (the ability to remove all cancerous tissue with clean margins).
This high-quality evidence signals a major shift in surgical oncology. It demonstrates that, in experienced hands, a minimally invasive approach can be used safely for even advanced tumors. This finding has the potential to allow more patients to benefit from the faster recovery associated with laparoscopic surgery without compromising their cancer control.
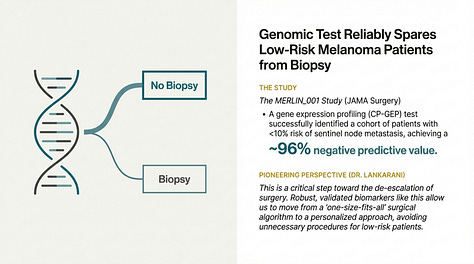
Finding 5: A Gene Test Can Spare Patients from Unnecessary Surgery
For many patients diagnosed with melanoma, the standard process includes a sentinel lymph node biopsy. This is a surgical procedure to remove and test the lymph nodes closest to the tumor to see if the cancer has started to spread. While it provides vital information, it is an invasive operation that many low-risk patients may n
ot need.
The MERLIN_001 study validated an innovative tool to solve this problem: a clinicopathologic gene expression profiling (CP-GEP) test. By analyzing the genetic profile of the primary tumor, this test can reliably identify a group of patients who have a very low risk (under 10%) of their cancer having spread to the lymph nodes.
The patient impact is profound. The study found the test achieved a negative predictive value of approximately 96%, meaning it is extremely accurate at identifying patients who do not have nodal disease. The adoption of this practice-changing tool could allow a significant number of low-risk patients to safely skip a needless operation altogether.
Conclusion: The Wisdom of Questioning
The findings from 2025 teach us that medical progress isn't just about questioning old beliefs, but about asking more precise questions. It's no longer enough to ask if a technology like robotics is better, but when and for whom. It's not about whether prehabilitation works, but which specific approach works for a given patient. This demand for nuance and high-quality evidence is what pushes the boundaries of care and ensures the operating room of tomorrow is truly better than the one today. As science continues to advance, which of today's medical certainties will become tomorrow's overturned assumptions?
To access additional details, please refer to the Surgical Pioneering Podcast Series application available at the following
https://Surgicalpioneer.codeadx.me